Internal Medicine
Our Program
The mission of the HES/Flowers Hospital Internal Medicine Residency Program is to provide quality education to future internists in the field of Internal Medicine and its subspecialties so as to graduate competent, empathetic physicians ready for autonomous practice or additional fellowship training in the field of their choosing. This mission is bolstered by three program aims:
- Residents will complete the majority of their training in community-based settings (Flowers Hospital, its ambulatory network, and private physicians’ offices) learning to work within a variety of team-based settings in suburban Alabama.
- Residents will actively participate in and contribute to active hospital and ambulatory clinic quality and process improvement initiatives to develop competency in practice-based learning, patient safety and quality improvement and systems-based practice.
- Residents will receive a balance of inpatient, outpatient and subspecialty experiences with the opportunity to individualize their clinical training experiences so as to maximize their skills in the specialty or subspecialty areas in which they intend to practice long-term.
Our Clinical Structure and Curriculum
Instead of structuring rotations as changing every month with a half-day of continuity clinic weekly, the program is taking a progressive approach, called an “X+Y Model.” The X+Y works within the constraints of the ACGME Internal Medicine requirements to separate the continuity clinic curriculum so that residents can be fully immersed in each rotational assignment. It allows, for example, a resident to work in the ICU for four weeks straight and never have to leave their critically ill patients to see patients in the clinic. Following those four weeks, they transition to the continuity clinic to begin a one-week rotation in outpatient medicine.
A Balanced Curriculum
The clinical training model is fairly evenly distributed between three types of learning – inpatient ‘bread and butter’ medicine (ED, Hospital Medicine, ICU), outpatient medicine (continuity clinic), and individualized learning experiences (electives). Resident selection of electives will be determined by their progression in the program, how they fare on in-training exams and evaluations on certain rotations. This allows residents to get more experience where there is opportunity to grow while bolstering their knowledge for the foundational practices of Internal Medicine (inpatient and outpatient).
The planned clinical training structure for all residents is outlined below (keeping in mind that these are totals and do not reflect the 4+1 scheduling structure):
PGY-1:
Inpatient Medicine: 4 (four-week blocks)
MICU: 2 (four-week blocks)
Night Float: 1 (four-week block)
Cardiology: 1 (four-week block)
Emergency Medicine: 1 (four-week block)
Continuity Clinic: 10 Weeks (in one-week blocks)
Neurology: 1 (four-week block)
Elective: 1 (four-week block)
PGY-2:
Inpatient Medicine: 2 (four-week blocks)
MICU: 1 (four-week block)
Medicine Consults for Ortho/Surg: 1 (four-week block)
GI/Night Float: 1 (four-week block)
Cardiology: 1 (four-week block)
Continuity Clinic: 10 Weeks (in one-week blocks)
Outpatient Medicine: 3 (four-week blocks)
Elective: 2 (four-week blocks)
PGY-3:
Inpatient Medicine: 2 (four-week blocks)
MICU: 1 (four-week block)
Medicine Consults for Ortho/Surg: 1 (four-week block)
GI/Night Float: 1 (four-week block)
Cardiology: 1 (four-week block)
Continuity Clinic: 10 Weeks (in one-week blocks)
Elective: 4 (four-week blocks)
Continuity of Care
ED and admitted patients without a PCP will be recommended for post-discharge follow-up at the continuity clinic. On the ambulatory-side, residents will be in the clinic for one week at a time every four weeks. To provide continuity over this five-week span, residents are assigned to a “team” of their peers so that each team has at least one resident team member in the clinic at any given time. The supervising faculty are those with a longstanding practice in the Dothan community and Flowers network.
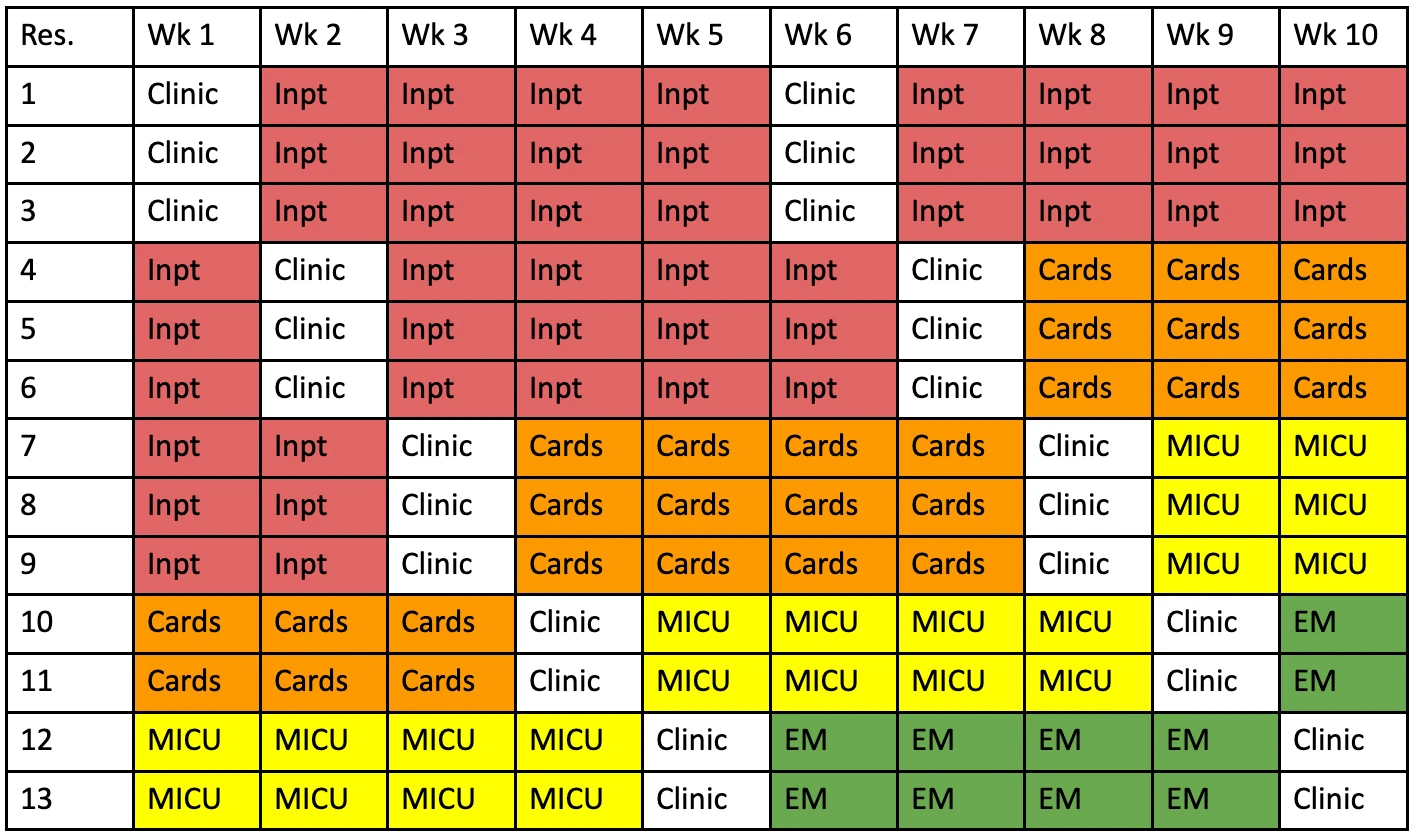
In the above example:
- Residents #1-3, #4-6, #7-9, #10-11, and #12-13 are always rotating into the continuity clinic at the same time. For ease of example, they also are rotating into the same four-week experience but that won’t actually be the case very often.
- You can also see that as Residents #1-3 transition to the “clinic” rotation, Residents #4-6 are staying through (both week 1 and week 6) to conserve continuity of care in the inpatient setting. As Residents #4-6 transition to the “clinic” rotation, Residents #7-9 provide that continuity in week 1 and Residents #1-3 are back providing that continuity in week 7.
From the outpatient, continuity clinic perspective, the +1 week of continuity clinic experience is designed as a +1 week with residents assigned to the same “care team” for their entire training duration. When residents are on this +1 week, they will have no inpatient duties or responsibilities.
- Residents will be assigned to continuity clinic every fifth week. Once that pattern is established, it continues for the duration of training.
- Residents will spend six half-days during that week in clinic in direct patient care, in addition to one-half day of administrative time for clinic messages/refills/callbacks, one half-day for academics/research, one half-day for the program-wide academic half-day, and one half-day in a subspecialty clinic.
- It is during this time and this experience we anticipate that residents will develop a long-term therapeutic relationship with the patient panel they care for as the identified Primary Care Provider (PCP).
- Given that treatment plans do not necessarily follow the same 4+1 pattern, the program is utilizing a “care team” model for assuring team-based continuity. As in, residents will be assigned to a care team with other peer residents so that at least one resident on the team is always in clinic and available to see the patient care team’s assigned panel, complete progress notes, follow-up with patients, specialists, and subspecialists while their resident-peers are immersed in their other inpatient clinical and educational experiences.
- When residents are switching into/out of the continuity clinic week, they will be trained to perform an outpatient hand-off to safely transition their patient panel’s treatment plan, including follow-up, to the next resident on the rotation.
- The example above demonstrates this hand-off process. Resident #1 can hand-off patient care of a patient that needs to follow-up in clinic to any of the residents on their care team (in this example, it’s Residents #1, #4, #7, #12) with whom their patient is scheduled for follow-up while they’re not in clinic. It is the expectation that the patient is “handed off” back to their PCP Resident Physician (Resident #1) for further follow-up.
Didactics, Conferences & Simulation Offerings
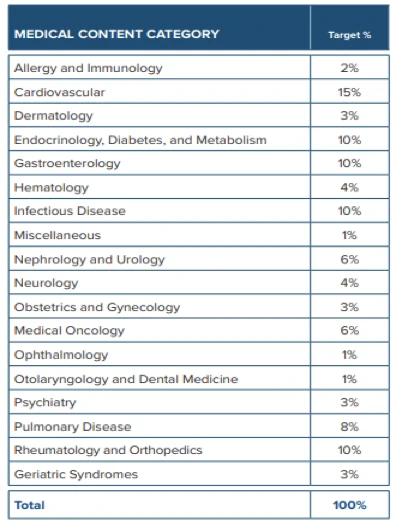 Instead of daily noon conference, residents will be attending a weekly didactic half-day that includes a balance of topics and presenter mix, resident v. faculty. Topics will be balanced in proportion to the ABIM’s Blueprint to the Board Exam.
The ABIM Blue Print allows the program the ability to assure the specialty-specific lectures provided to residents along an 18-month recurring curriculum provide the highest probability of assuring the educational needs of residents are met for board prep.
Instead of daily noon conference, residents will be attending a weekly didactic half-day that includes a balance of topics and presenter mix, resident v. faculty. Topics will be balanced in proportion to the ABIM’s Blueprint to the Board Exam.
The ABIM Blue Print allows the program the ability to assure the specialty-specific lectures provided to residents along an 18-month recurring curriculum provide the highest probability of assuring the educational needs of residents are met for board prep.
In addition to these topics, lectures will be given on social determinants of health, quality and process improvement, business of medicine, medical ethics, diversity and inclusion and other subjects determined needed and relevant by the Program Evaluation Committee.
Didactics will be in-person, onsite at Flowers Hospital taking place daily at noon, several days per week as well as a weekly half-day of education on Thursday afternoons.
Residents unable to attend can join virtually using Google Meet. Material related to all conferences such as journal articles, presentation material and handouts are stored in New Innovations under the Conference Module. Residents need only log in, navigate to the conference schedule and click the conference of interest to access, download and review the knowledge content they missed.
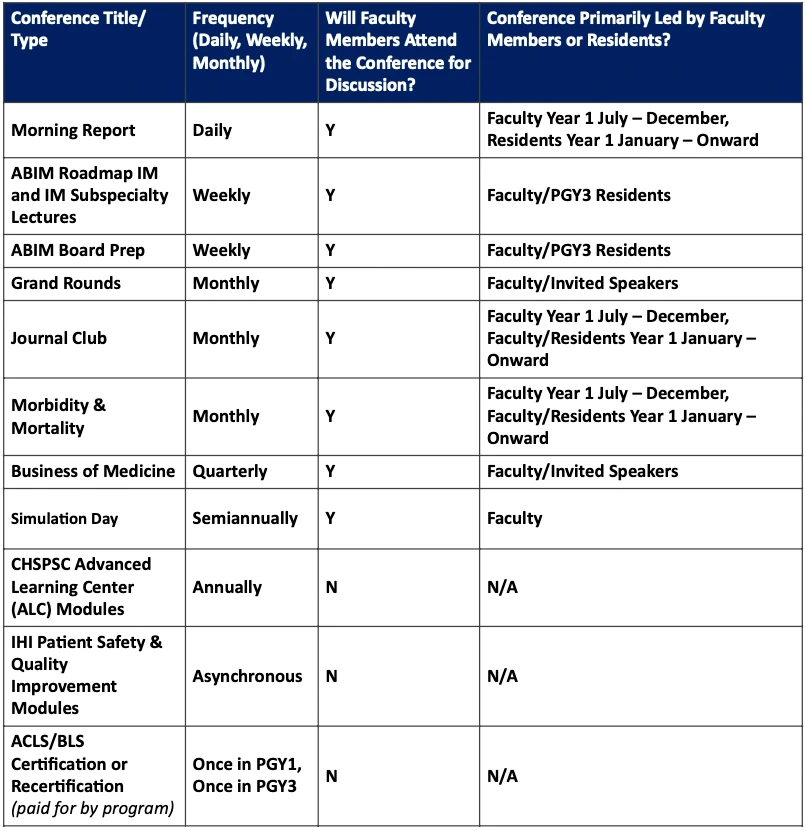
Scholarly Activity
The program requires residents complete at least two scholarly activity projects by end of training. This requirement and methods for satisfying it will be provided at Initial Appointment orientation. For example, PGY2 residents will be required to lead at least one Journal Club. PGY3 residents will be required to lead at least one Morbidity and Mortality conference. Residents will be encouraged and supported, however, in going above and beyond these minimum requirements. Residents whose work is accepted for poster or oral presentation will have up to $3,000 of the costs covered for conference attendance. Residents whose work is accepted for publication can request and may be granted additional administrative time to work on revisions to ensure success in publication.